Home Nutrition Support

Total Parenteral Nutrition
Total parenteral nutrition (TPN) is a method of providing nutrition to a person intravenously, bypassing the digestive system entirely. It is typically used when a person is unable to receive adequate nutrition through the digestive system, either due to a medical condition or because of a surgical procedure. TPN is generally provided through a central line or port-a-cath. It is possible to administer TPN via the peripheral route with special catered formulas. The current market for PN peripheral are SmofKabiven® Peripheral 1206ml and 1904ml & Numeta G13E 300ml.
The maximum rate of TPN we can administered is calculated by 2ml/kg/hr, typically 12-16hours to run overnight depends on the volume and calories prescribed. Some individuals may experience nausea/vomitting or stomach upset which can be prevented by administering drugs like proton pump inhibitor or anti-nausea injection prior to start of TPN. Some individual may required extra fluid to run concurrently with TPN if there is electrolytes imbalance showing signs of dehydration.
Our care team will check your bloods once or twice weekly, customise and optimize the nutrition treatment for you. We are 24/7 accessible and a guide on infusion pump alarm and troubleshooting will be taught on the commencement date. We have administered over thousands cases of home TPN and >99% of our patients have no major issue and were satisfied with the care rendered. Be rest assured and contact us for more details.
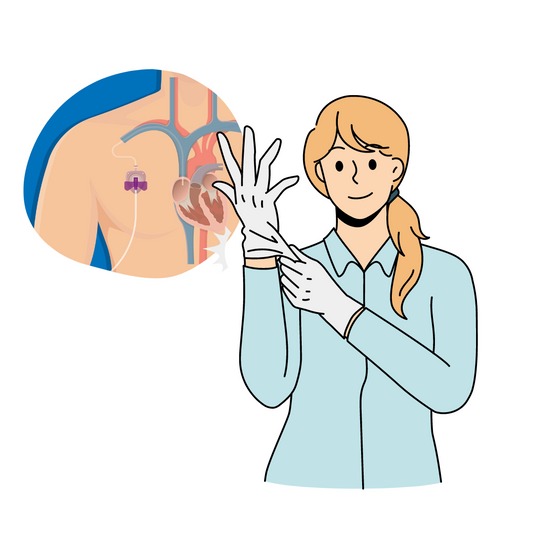
Nutrition via Port-a-Cath
A Port-A-Cath is a small medical device that is surgically implanted beneath the skin of a patient. It is a type of central venous catheter, which is used to provide direct access to the patient’s veins for long-term drug therapy, chemotherapy, or other treatments. The device is accessed by an experienced nurse or doctor, who uses a special needle to connect to the port. This allows medications and fluids to be administered more quickly and efficiently, avoiding the risk of infection associated with traditional IVs. The port can remain in place for months or even years, and the patient can be monitored to ensure the port is functioning properly.
Generally, it is recommended to flush the device every 4-6weeks with 1:1000 concentrated heparin with positive pressure technique to ensure that it does not become clogged and able to use for the next administration or blood taking.
Vickycares have all the required consumables and all our team nurses are competent to access to port-a-cath under aseptic technique.
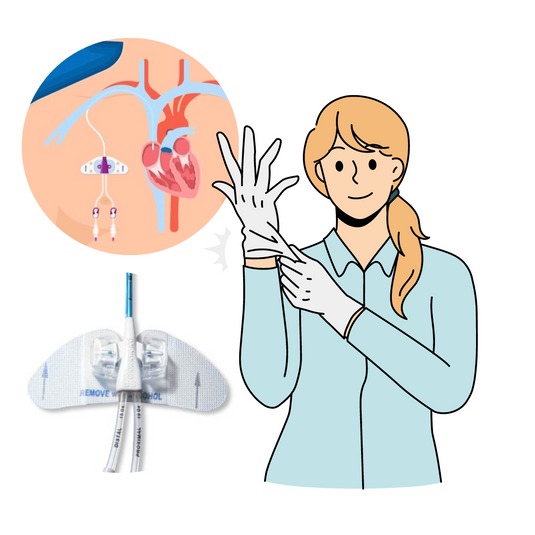
Nutrition via Central Venous Lines
Central venous access is a line inserted through a small incision made in the skin over the arm or chest under local anesthesia, then the line is routed through the vein and into the heart. It can be secured in place with a non-stitched dressing aka stat lock. Once the PICC line is in place, it can be used immediately to deliver nutrition.
We recommended 5-7 days of dressing change with chlorhexidine gluconate (CHG) impregnanted dressing to central venous line. Evidence studies have shown that it reduced the risk of catheter-related infection with CHG dressing instead of conventional adhesive film dressing (IV3000). A weekly flushing can be done together with the dressing change to keep the line patent
Vickycares have all the required consumables and our team nurses are competent to manage and provide caregiver teaching on dressing change and flushing. Consumables are available Click here to change this text
Nutrition in Advanced Diseases

It is common for loved ones with advanced illnesses to express their lack of desire to eat.
Reasons for loss of appetite may include:
- Changes in sense of taste or smell, making certain foods or drinks unpleasant.
- Discomfort caused by medication or treatment, such as constipation, nausea, vomiting, or bloatedness.
- The illness itself, such as cancer or organ failure, which may cause a loss of appetite.
- Pain from mouth sores, fungal infections, or dry mouth caused by radiation therapy.
- Chemical imbalances in the blood, such as high calcium levels, affecting normal bodily functions.
- Mood-related issues, such as depression, which can reduce appetite.
- Poorly controlled pain can further exacerbate low mood and reduce appetite.
- Advanced dementia can cause confusion and difficulty recognizing food, leading to refusal to eat, loss of interest in food, and holding food in the mouth instead of swallowing.
- Blockages in the body’s food passage may occur due to these factors.
- Muscle weakness or lack of teeth can cause difficulties in chewing and swallowing.
Difficulties swallowing
Difficulty swallowing can occur due to weakened or poorly coordinated muscles involved in the swallowing process. It’s essential to recognize the signs of difficulty swallowing in our loved ones, as it can increase the risk of choking on food or drink. If you notice any of the following common symptoms, it’s important to inform a doctor or nurse
- Coughing during/after most meals or some may presented with clearing of throat instead of cough
- Wet “gurgling” voice after drinking and/or while resting
- Coughing up a specific type of food/drink, e.g., coughing when eating rice but not porridge
- Prolonged chewing
- Breathlessness during/after a meal
- Holding food in the mouth and not swallowing
- Complaining of a sensation of something stuck in their throat
- Eating or drinking less than usual
Weight Loss
When an advanced illness affects nutrient processing in the body, it can result in the inability to build muscle or fat, even with a sufficient intake of food. This may cause significant weight and muscle loss to continue despite adequate food consumption.
Improving nutrition and the mealtime experience
In Singapore, food is often a way to show love and care towards our loved ones. It can be challenging to witness them losing weight despite our efforts and no longer enjoying meals that were specially prepared for them. While not all causes of appetite and weight loss are reversible, there are ways to improve their nutrition, comfort, and quality of life. One way is to understand their food preferences. Although they may have enjoyed certain types of food in the past, their preferences can change. By experimenting with different herbs, seasonings, and temperatures, we can enhance the flavor and make the meals more interesting. It’s crucial to listen to our loved ones, observe their responses to food and drinks, and be receptive to their changing feedback.

Maintaining oral hygiene is essential to keep the mouth fresh and clean
- Brush and rinse the mouth daily using an ultra-soft toothbrush or an oral swab stick
- Use regular mouth rinses or a homemade mouth rinse with salt dissolved in warm water to keep the mouth fresh
- Consume flavored ice chips or semi-frozen pineapple to maintain a fresh mouth
- Look out for mouth ulcers, sores, or patches of red or white which may indicate a fungal infection and inform the doctor or nurse if noticed
- Remove and clean dentures before and after every meal to maintain oral hygiene
- Keep a small sipper bottle of their favorite drinks by their bedside to allow frequent sips or a small spray bottle to moisten their mouth
- If unable to drink or swallow, use an oral swab stick to gently clean the mouth and apply moisturizing mouth gel to keep it clean and moist

Making mealtimes enjoyable and easier for your loved one is crucial for their overall well-being.
Here are some tips to make it happen:
- Create a pleasant dining environment by using their favourite tablecloth or placemat, playing calming music or showing family photos.
- Ensure that they are seated comfortably and at a suitable height for eating.
- Consider using utensils that are easy to grip and use, such as bendable or weighted utensils.
- Serve small and frequent meals throughout the day, rather than three large meals, to avoid overwhelming your loved one.
- Offer a variety of food choices and textures that are easy to chew and swallow.
- Allow enough time for meals, and avoid rushing or forcing them to eat.
- Engage in conversation during mealtimes to make it a more social and enjoyable experience.
- Be mindful of any dietary restrictions or preferences and adjust accordingly.
- Consider consulting with a dietitian or nutritionist to ensure that your loved one is getting adequate nutrition.
- Offer positive reinforcement and encouragement to your loved one, such as praising them for eating well or trying a new food.

Assisting and pacing your loved one during mealtimes can help ensure their safety and comfort.
Here are some ways to do it:
- Sit with your loved one during meals to provide assistance as needed, such as cutting food into small pieces or opening containers.
- Allow them to eat at their own pace and avoid rushing them.
- Provide small sips of fluid between mouthfuls of food to help them clear the food int he mouth
- Offer assistance with utensils or feeding if needed.
- Monitor their chewing and swallowing to ensure that they are not experiencing any difficulty or discomfort.
- Pay attention to their body language and any signs of fatigue or discomfort.
- Allow frequent breaks during meals if needed.
- Be patient and understanding, as eating can become a challenging and tiring activity for those with difficulty swallowing or other medical conditions.
- Consult with a healthcare professional, such as a speech therapist, for further guidance on how to assist and pace your loved one during meals.

Various ways to make meals more visually appealing and interesting for your loved one.
- Incorporate a variety of colourful ingredients in a dish, such as mixing diced carrots and mashed potatoes with a side of broccoli.
- Use contrasting colours of food and crockery, such as serving porridge in a red bowl instead of a white bowl.
- Use various kitchen tools, such as ice cream scoops, muffin cups, or cookie cutters, to shape blended or minced food, making it more visually appealing and interesting.

Serve small meals or snacks throughout the day
- Encourage your loved one to decide when and what they would like to eat
- They may prefer 5 to 6 small meals a day instead of 3 large meals
- Small servings may be less intimidating and easier to tolerate
- Offer additional food if they are still hungry
- If nausea is present, serve the prescribed nausea medication at least 30 minutes before a meal, or as advised by the doctor.

Making every mouthful of food count is important to ensure that your loved one is receiving adequate nutrition.
- Add sesame oil, egg, fish or tofu to porridge to increase calorie and protein content.
- Add peanut butter or tuna biscuits to meals.
- Incorporate oral nutritional supplements to milkshakes.
- Provide high-calorie, high-protein snacks such as red or green bean soup, sesame paste, bubur cha cha, bao, and beancurd.
- Offer nourishing fluids like soy milk, full cream or flavoured milk, oral nutritional supplements, fruit smoothies, and yoghurt drinks.
- Add milk, ice cream, or honey to beverages to increase calorie and nutrient content.

Avoiding excessive fluid intake during meals is crucial for digestion and nutrient absorption.
- Fluid, especially fizzy drinks, can cause your loved one to feel full or bloated quickly.
- Unless your loved one is taking fluid meal replacements, only offer sips of fluids during meals to clear the palate.
- Allow your loved one’s body to guide the amount of food and fluids to be consumed.
- Force-feeding can cause distress, physical discomfort, or pain.
- The goal of eating is to maximize enjoyment and eat as much as your loved one is able to tolerate, even if it means only a small amount for taste.
Use a suitable consistency
Food and fluid consistency can have a significant impact on the ease of swallowing. A speech therapist or nurse can help you determine the most appropriate consistency for your loved one’s needs. It’s crucial to consult with a healthcare professional to ensure that your loved one is receiving safe and adequate nutrition.
